Fungi: They’re Everywhere!
MIC and MFC Testing against Filamentous Fungi
Fungal spores are commonplace in households and many work environments. In small quantities to healthy people, there are no adverse effects. In large quantities or in immunocompromised people, it can cause serious complications. According to the Center for Disease Control (CDC), the common indoor molds include Cladosporium, Penicillium, Alternaria and Aspergillus. Each of these groups of mold has the potential to cause infection, but will more likely cause allergic reactions.1,2,3 Molds and fungi are found everywhere, in the water, soil, plants, on the skin, most surfaces and in the air. It thrives in humid, warm and damp locations like the bathroom.
Of the four common indoor molds, Aspergillus is most likely to cause fungal infections. Unfortunately, Aspergillosis is unreportable so the number of people who contract this mold per year is unknown. Among stem cell transplant recipients, however, it is the most common cause of fungal infection, and it is the second-most common among organ transplant recipients. 4,5
A familiar fungal infection is onychomycosis, also known as fungal nail infection. Onychomycosis is found in 10% of the general population, half of which are 70 or older. 6 Dermatophytes, Trichophyton rubrum and Trichophyton mentagrophytes, are the major culprits. However, onychomycosis patients have also been cultured with non-dermatophytic filamentous fungi, such as Scopulariopsis, Aspergillus, Alternaria and Fusarium. Onychomycosis occurs more commonly in toenails than fingernails. People with fungal nail infections can develop tinea pedis, more frequently known as athlete’s foot. Vice versa, people with athlete’s foot can develop onychomycosis. Both infections are treated with antifungals, orally for onychomycosis and topically for tinea pedis. Onychomycosis may take up to a year with the current antifungal treatments for the infection to completely go away.5
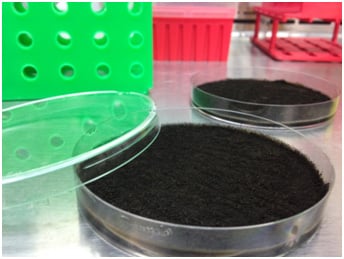
The Clinical and Laboratory Standards Institute (CLSI) has developed a protocol for testing antifungal susceptibility against filamentous fungi using a minimum inhibition concentration (MIC) assay. The filamentous fungi are grown on potato dextrose agar at 35°C. Aspergillus and most other fungi need to be grown for 7 days. However, Fusarium has to be incubated at 35°C for 2-3 days prior to lowering the temperature to 25-28°C for an additional 4-5 days. The fungal inoculum will be made by adding 0.9% saline solution to the fungal plates and gently scraping them. The inoculum will be diluted to about 104 CFU/mL and added to the testing agent that is at twice the intended concentration. Microtiter plates will be incubated at 35°C without agitation. Rhizopus will only be incubated for 21-26 hours while all other fungi will be incubated for 46-50 hours. If working with Pseudallescheria boydii, the MIC plate will need to be incubated for 70-74 hours.
Reading the results of the MIC plate is very similar to reading yeast MIC plates because there is also a scoring system. This system defines that testing against flucytosine, fluconazole and ketoconazole’s readings will be read where 50% of growth is reduced (score of 2). With other antifungals, the MIC would be at the lowest concentration to present an optically clear well, a score of 0.
Scores Visibility
0 Optically clear/absence of growth
1 Slight growth/25% of the growth control
2 Prominent reduction in growth/50% of the growth control
3 Slight reduction in growth/75% of the growth control
4 No reduction of growth
The minimum fungicidal concentrations (MFC) can also be determined after reading the MIC plates. From each concentration that presents an optically clear well, 20 µL is plated onto Sabouraud dextrose agar (SDA) and incubated at 35°C. This is also repeated for the growth control well. Plates are incubated for about 48 hours. The MFC is determined to be the lowest concentration at which ≤ 3 colonies grow on an SDA plate.9
Antifungal susceptibility assays predict therapeutic potential of prospective new agents. Emery Pharma offers this MIC and MFC assay for testing potential antimycotic drugs. EPS also provides services for biofilm and resistance profiling. For more information and a quote, please contact us at 510-899-8828.
- Bouziane H, Latge JP, Fitting C, Mecheri S, Lelong M, David B. “Comparison of the allergenic potency of spores and mycelium of Cladosporium.” Allergologia et Immunopathologia. 33.3 (2005):125-130.
- Shen HD, Tam MF, Tang RB, Chou H. “Aspergillus and Penicillium allergens: focus on proteases.” Current allergy and asthma reports. 7.5 (2007):351-356.
- Perzanowski MS, Sporik R, Squillace SP, Gelber LE, Call R, Carter M, Platts-Mills TA. “Association of sensitization to Alternaria allergens with asthma among school-age children.” The Journal of Allergy and Clinical Immunology. 101.5 (1998):626-632.
- Kontoyiannis DP, Marr KA, Park BJ, Alexander BD, Anaissie EJ, Walsh TJ, et al. Prospective surveillance for invasive fungal infections in hematopoietic stem cell transplant recipients, 2001-2006: overview of the Transplant-Associated Infection Surveillance Network (TRANSNET) Database. Clinical Infectious Disease. 50.8(2010):1091-1100.
- Pappas PG, Alexander BD, Andes DR, Hadley S, Kauffman CA, Freifeld A, et al. Invasive fungal infections among organ transplant recipients: results of the Transplant-Associated Infection Surveillance Network (TRANSNET). Clinical Infectious Disease. 50.8(2010):1101-1111.
- Westerberg, DP and MJ Voyack. “Onychomycosis: Current trends in diagnosis and treatment.” American Family Physician. 88.11 (2013): 762-770.
- Elewski, B. “Onychomycosis: Pathogenesis, Diagnosis, and Management.” Clinical Microbiology Reviews. 11.3 (1998): 415-429.
- Garcias-Martos P, Dominiguez I, Marin P, Linares M, Mira J, Calap J. “[Onychomycoses caused by non-dermatophytic filamentous fungi in Cadiz].” Enfermedades infecciosas y microbiologia clinica. 18.7 (2000): 319-324.
- Espinel-Ingroff A, Fothergill A, Peter J, Rinaldi MG, Walsh TJ. “Testing Conditions for Determination of Minimum Fungicidal Concentrations of New and Established Antifungal Agents for Aspergillus spp.: NCCLS Collaborative Study.” Journal of Clinical Microbiology. 40.9 (2002):3204-3208.