Testing Antimicrobial Activity and Cytotoxicity of Wound and Skin Cleansers
Chronic non-healing wounds, such as venous ulcers, diabetic ulcers, and pressure ulcers, cause tremendous patient suffering. Treatment of such wounds presents a serious unmet medical need. Strategies that optimize tissue repair have evolved with advances in understanding of the wound healing process [1]. Infection control in chronic wounds is an important part of these strategies. Evidence shows that a bacterial burden of 10⁶ microorganisms or more per gram of tissue seriously impairs healing. Bacteria may stimulate persistent inflammation, leading to the production of inflammatory mediators and proteolytic enzymes. Among many other effects, this causes extracellular matrix (ECM) degradation and inhibition of re-epithelialization.
Recently, there has been increased interest in the role of bacterial biofilms in impaired wound healing. Epithelial advancement, another critical component of wound healing, requires the activity of fibroblasts and keratinocytes—which may be hampered by aggressive and toxic wound and skin cleansers. When such products are used, not only are bacteria killed, but epithelial cells can be damaged as well. An ideal wound cleanser provides periodic reduction of bacterial contamination and removal of necrotic tissue and biofilm debris without adversely impacting cellular activities vital to the wound healing process. Therefore, important steps in a comprehensive strategy for evaluating wound care products include testing their antimicrobial efficacy and potential cytotoxicity for relevant cell types.
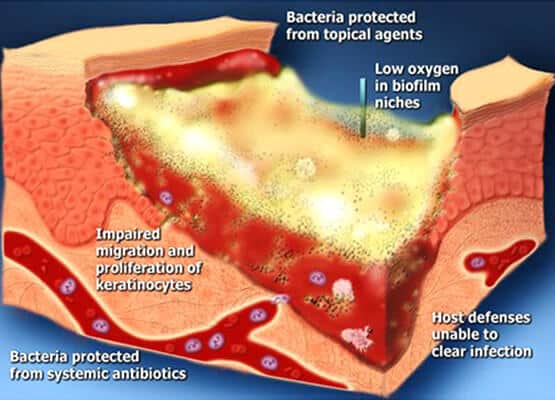
Figure 1. Bacterial biofilm plays a significant role in delaying wound healing.
Emery Pharma offers several models for cytotoxicity testing and utilizes a panel of microbial strains to evaluate antimicrobial activity of wound cleansers. In the example shown in Table 1, we determined the non-cytotoxic, safe concentration of several important and widely used skin and wound cleansers using a cytotoxicity assay with L929 mouse fibroblasts. We then compared the microbicidal activity of these cleansers at their non-cytotoxic concentration against Methicillin-Resistant Staphylococcus aureus (MRSA) ATCC 33591. Cytotoxicity was evaluated using modified methods described by Wilson et al. [2]. Cells were cultured in 96-well plates to approximately 70% confluency before being exposed to various cleansers. Cleansers were aspirated off the wells after 30 minutes of exposure at 37°C. Cells were then incubated in fresh media overnight before cell viability was determined using the CellTiter 96 cell proliferation assay (Fig. 2). Cleansers were serially diluted 1:10 with PBS.
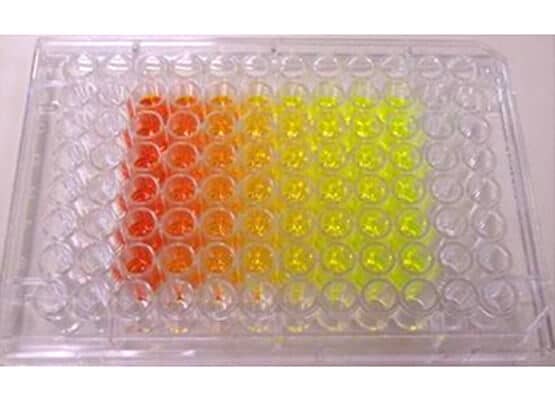
Figure 2. Testing cytotoxicity by CellTiter 96 cell proliferation assay
|
Agents Tested |
Nontoxic dilution |
Time to 4 Log10 Kill |
|
Formulation A |
100 |
>24 hrs |
|
Formulation B |
10-1 |
30 min |
|
Formulation C |
10-1 |
>24 hrs |
|
Formulation D |
10-1 |
<1 min |
Table 1. Toxicity index and antibacterial time-kill kinetics of cleansers.
Each cleanser was serially diluted 1:10 with PBS, and each dilution was tested for cytotoxicity until cell response matched that of PBS-exposed controls.
Formulation A was found to be the least toxic to fibroblasts, requiring no dilution to maintain viable cells. Several formulations (B, C, D) required a 10-fold dilution.
The time-kill assay is a measure of how long it takes for an antimicrobial wound product to achieve a 4-log (99.99%) kill of a defined microbial inoculum. This assay was conducted using modified Clinical and Laboratory Standards Institute (CLSI) methods. A standard inoculum of MRSA ATCC 33591 was grown, centrifuged, and resuspended to approximately 10⁸ CFU/mL before incubation with the cleansers at their non-cytotoxic dilution for 1, 5, 15, 30, and 60 minutes, as well as 4 hours and 24 hours. Ten-fold serial dilutions of the cleanser-inoculum mixtures were plated on TSA, incubated overnight at 37°C, and colony-forming units (CFUs) were counted (Fig. 3). Examples of these studies are shown in Fig. 4.
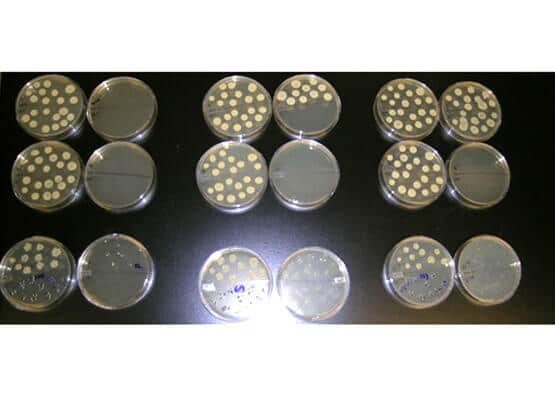
Figure. 3. Bacteria plated for CFU counts
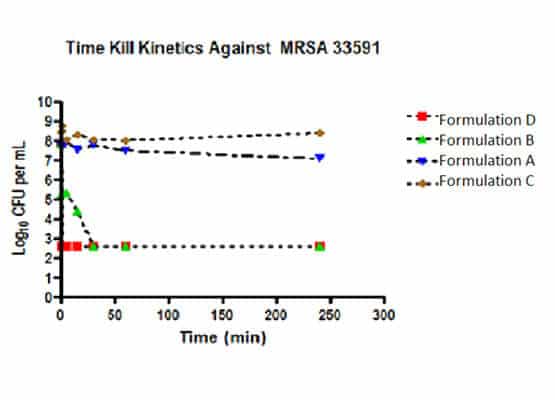
Figure 4. The time to kill at the non-toxic dilution of Formulation D (10-fold dilution) was less than 1 min, followed by Formulation B (10-fold dilution) at 30 minutes. Formulations A and C showed no log reduction at 24 hours.
These studies are useful to clinicians developing advanced wound care strategies and to researchers wishing to expand in vitro testing methods to evaluate the potential cytotoxic and bactericidal effects of agents used for wound cleansing. This study demonstrates that many commercial wound and skin cleansers (Fig. 5) may be toxic to fibroblasts—one of the key cells in wound repair—and suggests that these cleansers might also affect other cell types involved in healing. When diluted to cell-safe concentrations, most cleansers lost significant antibacterial activity, as reflected by the extended time required to inhibit growth of S. aureus, while some products stood out for maintaining both low toxicity and effective antimicrobial activity.

Figure 5. Wound and skin cleanser products
Emery Pharma also offers a wide range of microbiology laboratory services including resistance profiling , antimicrobial susceptibility testing, antibiotic sensitivity testing, and custom biofilm model assays, all of which can be tailored to your specific product or research needs. Contact us today to learn how our expertise in wound care testing can advance your research and product development!
About the Author
Originally authored by Dr. Dmitri Debabov. This article was reviewed and updated on June 6, 2025 by Dr. Janet Liu, current Director of Biology.
References:
1. Grotendorst GR, Pencev D, Martin GR, Sodek J. Molecular mediators of tissue repair. In: Hunt TK, Heppenstall RB, Pines E, Rovee D, eds. Soft and Hard Tissue Repair. Biological and Clinical Aspects (Surgical Sciences Series). Vol 2. New York: Praeger; 1984.
2. Wilson JR, Mills JG, Prather ID, Dimitrijevich SD. A toxicity index of skin and wound cleansers used on in vitro fibroblasts and keratinocytes. Advances In Skin & Wound Care 2005; 18:373 – 378
